Arrhythmogenic Ventricular Cardiomyopathy (ARVC) in Dogs
Table of contents
- Arrhythmogenic Ventricular Cardiomyopathy (ARVC) in Dogs
- Introduction to ARVC
- What is ARVC?
- The Causes Behind ARVC
- Symptoms of ARVC
- Implications of ARVC
- Diagnosing ARVC
- Treatment and Management
- Breeding Ethics and Genetic Testing
- Diving Deeper into Heart Health
- How the Heart Pumps
- Conclusion
- Additional Curious Questions
- What regulates the pace and frequency at which signals are transmitted?
- How does the brain increase heart rate?
- How does the brain decrease heart rate?
- Can the heart beat without the brain?
- Why does irregular heart rate, result in sudden cardiac death?
- Why does irregular heart rate result in cough?
- Why does irregular heartbeat results in blood clots?
- What is meant by Turbulent Blood Flow?
- Thank You
- Fun Facts
When we think of heart health, our minds often jump straight to humans, but did you know that man’s best friend can suffer from heart conditions too? Today, we’re dipping our toes into the world of Arrhythmogenic Ventricular Cardiomyopathy (ARVC) in dogs—a complex condition that requires a keen understanding for those who love and care for these animals.
The material in this articles are for educational purposes only. If you suspect that your dog have ARVC or any other medical conditions, please contact a professional for further assessment!
Introduction to ARVC
Interestingly, while not common in breeds like the Aussie Shepherd, ARVC is a condition that should not be mistaken by pet owners and breeders for Hemangiosarcoma (HSA) cancer.
While ARVC might not ring alarm bells as often in breeds like the Aussie Shepherd, its presence is notably concerning and demands careful attention to distinguish it from other severe conditions such as Hemangiosarcoma (HSA) cancer.
The challenge lies in the fact that ARVC and HSA both can trigger sudden collapsing episodes in dogs, a symptom that muddies the waters for pet owners trying to understand their pet’s health issues. This overlap emphasises the importance of accurate diagnosis, as ARVC, while a non-curable heart disorder, can be managed with early detection and the right care approach to slow its progression and maintain a quality life for affected dogs.
Here, we emphasize again the importance of checking in with a veterinary professional if you suspect that your furry companion is suffering from a health condition, as veterinary professionals has undergone rigorous training that would allow for them to provide an accurate diagnosis and remove unnecessary guesswork when it comes to your pet’s well being!
What is ARVC?
At its core, ARVC is a genetic condition predominantly seen in certain dog breeds. It affects the myocardium, the muscular wall of the heart, causing parts of it to be replaced by fibrous tissue and fat. This change disrupts the heart’s normal electrical impulses, leading to irregular heart rhythm: arrhythmias.
The Causes Behind ARVC
The exact cause of ARVC in dogs remains a bit of a mystery but is believed to have a strong genetic component. Certain breeds are predisposed to the condition, highlighting the importance of genetic testing and responsible breeding practices.
Genetic Predisposition
The likelihood of a dog developing ARVC is significantly influenced by their genetic makeup, with certain breeds being more predisposed to this condition. Breeds like the Boxer are particularly at risk, illustrating the hereditary nature of ARVC. This underlines the critical role of genetic testing for breeding dogs to identify carriers of the genes associated with ARVC and to help minimize the spread of this condition through careful breeding decisions.
Inflammatory Processes

While the genetic aspect of ARVC is well acknowledged, the role of inflammatory processes cannot be overlooked. Conditions that cause chronic inflammation in the body may exacerbate or contribute to the development of ARVC by affecting the heart muscle. This link suggests that maintaining overall health and promptly addressing any inflammatory conditions can be key in managing the impact of ARVC in predisposed breeds.
Environmental Factors

Environmental factors, though not as directly related to the onset of ARVC as genetic predisposition, can influence the course of the disease. Factors such as excessive exercise, improper diet, and stress can aggravate the symptoms of ARVC or accelerate its progression. Awareness and control of these environmental aspects are crucial in managing a dog’s condition, offering them a better quality of life despite their diagnosis.
Symptoms of ARVC
Many dogs with ARVC may not show signs initially, making early detection challenging. Symptoms can include weakness, exercise intolerance, coughing, difficulty breathing, fainting episodes, and even sudden collapse due to arrhythmias like ventricular tachycardia and fibrillation:

Weakness:
Dogs affected by ARVC may exhibit overall lethargy or sudden bouts of weakness. This can affect their exercise routine and daily activities, making them less eager to engage in play or walks.
Exercise Intolerance:
One of the hallmark symptoms, dogs with this condition may struggle or become quickly exhausted during activities they previously enjoyed. Monitoring changes in how your dog responds to exercise is crucial.
Coughing:
Persistent coughing can arise as the heart’s ability to pump efficiently is compromised, potentially leading to fluid accumulation in the lungs.
Difficulty Breathing:
Breathing may become laborious if there is increased pressure in the heart or fluid buildup in the lungs, causing distress and rapid breathing even at rest.
Fainting Episodes:
Sudden loss of consciousness (syncope) may occur due to irregular heartbeats that disrupt blood flow to the brain. These episodes can be particularly alarming and warrant immediate veterinary attention.
Sudden Collapse:
In severe cases, dogs can experience acute collapse, often triggered by vigorous activity, due to dangerous heart rhythms that can be fatal if not promptly addressed.
Implications of ARVC
Understanding the implications of Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC) in dogs is vital for managing their health and well-being. This condition not only affects the physical state of the heart but also has broader effects on a dog’s overall quality of life and longevity.

Impaired Conduction:
Impaired conduction refers to the heart’s compromised ability to transmit electrical signals effectively. In dogs with ARVC, this can lead to irregular heart rhythms, adversely affecting cardiac efficiency and overall health. Timely management and monitoring are essential to mitigate the risks associated with impaired conduction, ensuring the heart can maintain its critical functions.
Increased Risk of Sudden Cardiac Death:
ARVC significantly raises the risk of sudden cardiac death (SCD) in dogs. This drastic event usually results from severe ventricular arrhythmias, where the heart cannot pump blood effectively, leading to sudden collapse and potentially death. Understanding and managing the risks associated with ARVC can help in preventing such outcomes by instituting appropriate interventions.
Symptoms of Heart Dysfunction:
The progression of ARVC may manifest in noticeable symptoms indicative of heart dysfunction, including lethargy, reduced exercise capability, and signs of heart failure like coughing and difficulty breathing. Recognising these symptoms early can prompt necessary evaluations and treatments, improving life quality and longevity for the affected dogs.
Increased Risk of Thromboembolism:
Thromboembolism, the obstruction of blood vessels by blood clots, presents an increased risk in dogs with ARVC due to the potential for blood pooling and clot formation as a result of abnormal heart rhythms. Preventative care, including blood thinners or other medical interventions, may be necessary to reduce this risk and safeguard the dog’s circulatory health.
Progressive Cardiac Dysfunction:
ARVC can lead to a downward spiral in cardiac health, where the heart’s ability to function deteriorates over time. This progressive cardiac dysfunction can severely impact a dog’s stamina, comfort, and survival. Management strategies can include medications, lifestyle adjustments, and regular veterinary check-ups to slow the progression of the disease and maintain the best possible quality of life.
Diagnosing ARVC
Detecting ARVC involves a combination of observing clinical signs, a thorough physical examination, and specific diagnostic tests such as ECG, echocardiography, and Holter monitoring. In some cases, genetic testing can provide valuable insights.

The outlook for dogs with ARVC varies. Some may lead relatively stable lives with proper management, while others may face a progressive decline in heart function. Regular veterinary check-ups are crucial for catching and managing the condition early on.
Early detection of ARVC is not just beneficial—it’s crucial for ensuring a dog’s quality of life remains as high as possible. By identifying the condition in its nascent stages, treatment can begin sooner, potentially slowing the progression of cardiac dysfunction and allowing for a more tailored and effective management plan.
Treatment and Management
While there’s no cure for ARVC, management strategies focus on controlling arrhythmias and supporting heart function through medication, lifestyle modifications, and regular veterinary check-ups. Key treatments or management strategies include:

Antiarrhythmic Drugs:
These medications are vital in managing ARVC as they help to stabilize the heart rhythm, reducing the frequency and severity of arrhythmias. For dogs diagnosed with ARVC, antiarrhythmic drugs can significantly improve the quality of life by minimizing the risk of sudden cardiac events.
ACE Inhibitors or Beta-Blockers:
ACE inhibitors can enhance heart function by relaxing blood vessels and reducing the workload on the heart, while beta-blockers slow down the heart rate and lessen the force of the heart’s contractions. Both types of medication play a crucial role in managing symptoms and slowing disease progression in dogs with ARVC.
Lifestyle Modifications:
Adjustments to a dog’s lifestyle, such as managing exercise routines to avoid overexertion, maintaining a healthy weight, and feeding a well-balanced diet, are essential. These changes can help mitigate the symptoms of ARVC and support overall heart health, making them a fundamental aspect of long-term care for affected dogs.
Breeding Ethics and Genetic Testing
Breeders also play a pivotal role in combating the prevalence of ARVC. By maintaining meticulous health records and conducting genetic testing, breeders can make informed decisions that prioritise the health and welfare of future generations, ensuring ethical breeding practices. Engaging in such proactive measures not only protects the lineage but also contributes to the overall well-being of the breed.
Given ARVC’s genetic links, responsible breeding practices are vital. Genetic testing can identify carriers of gene mutations associated with ARVC, providing a powerful tool for reducing the disease’s prevalence in susceptible breeds.
Diving Deeper into Heart Health
Understanding ARVC in dogs requires a basic knowledge of how the heart works, including the importance of electrical conductivity and what happens when it goes awry. Our hearts—and our dogs’ hearts—are incredible machines, but they need the right care and attention to keep beating strong.

At the core of it all, the heart is a powerful muscle that pumps blood throughout the body, supplying oxygen and nutrients to tissues and removing carbon dioxide and other wastes. This continuous cycle begins when the heart’s right side receives deoxygenated blood and pumps it to the lungs for oxygenation. Oxygen-rich blood then returns to the heart’s left side before being circulated to the rest of the body.
How the Heart Pumps
This process hinges on an intricate electrical system that ensures the heart muscles contract in a synchronized manner, maintaining a steady rhythm and rate. Without this precise coordination, the heart’s efficiency can falter, leading to potential health issues. For a deeper understanding of this vital organ’s function and importance, click here.
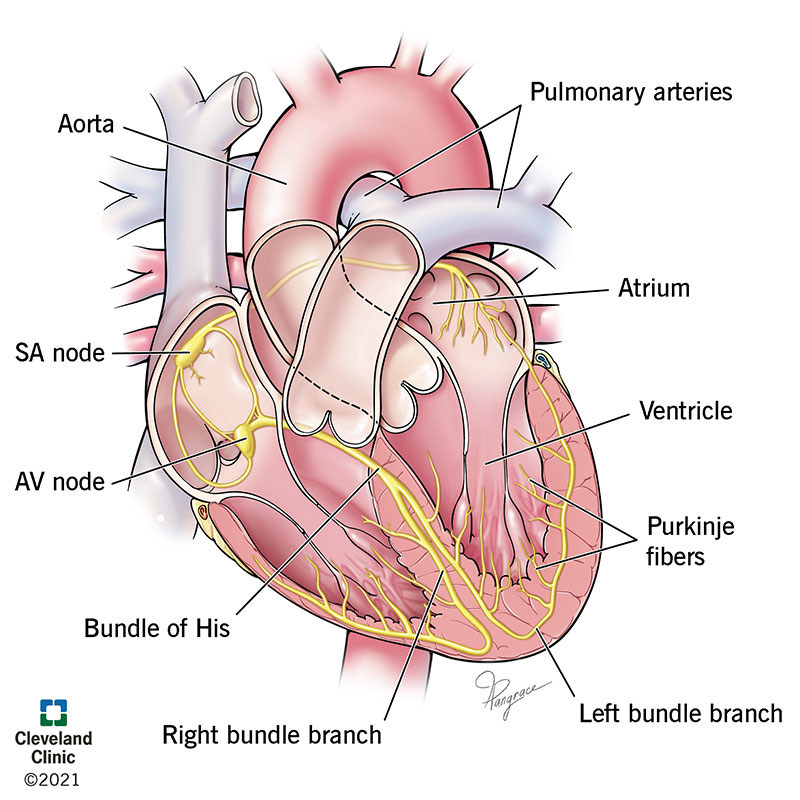
Sinoatrial (SA) node
The heart’s ability to pump efficiently relies on a specialized electrical system, a true marvel of biological engineering. At its foundation is the sinoatrial (SA) node, often referred to as the heart’s natural pacemaker. This cluster of cells, located in the right atrium, generates electrical impulses that initiate each heartbeat. These impulses spread throughout the atria, prompting them to contract and push blood into the ventricles.
Atrioventricular (AV) node
Following the SA node’s cue, the atrioventricular (AV) node, situated between the atria and ventricles, acts as a gatekeeper that slightly delays the electrical signal. This pause ensures the atria have time to fully contract before the ventricles begin their contraction, thus allowing for efficient blood flow. After this brief delay, the signal moves to the bundle of His and then through the Purkinje fibers.
Bundle of His and Purkinje Fibers:
This network, which includes the Bundle of His and Purkinje fibers, is responsible for distributing the electrical impulse evenly across the ventricles, causing them to contract in unison.
The Bundle of His is a collection of heart muscle cells specialized for electrical conduction. These cells transmit the electrical impulses from the atrioventricular node, down through the interventricular septum before branching into the Purkinje fibers. The Purkinje fibers further spread the impulse throughout the ventricles, ensuring they contract simultaneously. This coordinated contraction is vital for efficiently propelling blood out of the heart to the lungs for oxygenation, and subsequently to the rest of the body, maintaining effective circulation.
This electrical orchestration ensures the heart works as an effective pump, maintaining the vital circulation of blood necessary for life. Understanding these mechanisms highlights the importance of electrical conductivity in heart health and the potential consequences when this delicate system is disrupted.
Conclusion
ARVC in dogs is a complex condition that poses significant challenges but also highlights the importance of genetic understanding and responsible pet care. Whether you’re a pet owner, breeder, or simply a dog lover, staying informed about conditions like ARVC is crucial for the well-being of these beloved animals.
Remember, early detection and intervention are key. By keeping a close eye on our furry friends and working with veterinary professionals, we can manage conditions like ARVC and ensure our dogs live happy, healthy lives.
Additional Curious Questions
In exploring heart health, several curious questions arise. For instance, what controls the rhythm and frequency of the heart’s electrical signals? And can the heart beat without the brain? These questions touch on the intricate balance of hormonal control and the heart’s somewhat autonomous nature.
What regulates the pace and frequency at which signals are transmitted?
The rhythm and frequency of the heart’s electrical signals are primarily controlled by the sinoatrial (SA) node, often referred to as the heart’s natural pacemaker. However, beyond this intrinsic control system, the heart’s functioning is significantly influenced by hormonal signals, primarily those released from the adrenal glands, such as adrenaline (epinephrine) and noradrenaline (norepinephrine), in response to the brain’s perception of stress or physical demands.
How does the brain increase heart rate?
When the brain detects a need for increased blood circulation – whether due to physical activity, emotional stress, or other factors – it signals the adrenal glands to release these hormones. These hormones bind to receptors on the heart cells, causing an increase in heart rate and force of contraction. This mechanism ensures that more oxygen-rich blood is circulated to the organs and muscles that need it most.
How does the brain decrease heart rate?
Furthermore, the vagus nerve, part of the parasympathetic nervous system, releases acetylcholine, a neurotransmitter that acts to slow down the heart rate when the body is at rest or in a state of relaxation, highlighting a sophisticated balance between the sympathetic and parasympathetic nervous systems in controlling heart function. This interplay of hormonal signals and nervous system inputs is crucial for adapting heart activity to the body’s varying needs, ensuring it operates effectively in a wide range of situations.
Can the heart beat without the brain?
Indeed, the heart can maintain its rhythm without direct commands from the brain, thanks to its unique, built-in electrical system. Central to this system is the sinoatrial (SA) node, which autonomously generates electrical impulses, prompting the heart to beat. This capability demonstrates the heart’s remarkable independence; it can continue to function even in the absence of brain activity.
This phenomenon underlies the principle of heart transplants, where the donor heart, once connected to the recipient’s blood supply, spontaneously begins to beat. The heart’s intrinsic capability to beat highlights its profound resilience and underscores the sophisticated evolution of human physiology.
Additional fun facts regarding how the independence of the heart function from brain activity serves as a crucial role in keeping organs healthy and alive whilst pending transplant! Curious? Click here to check it out!
Why does irregular heart rate, result in sudden cardiac death?
An irregular heart rate disrupts the heart’s ability to pump blood efficiently, which is critical for delivering oxygen to the body’s tissues and organs. When arrhythmias occur, such as ventricular tachycardia or ventricular fibrillation, the heart’s rhythm becomes too rapid or chaotic to maintain effective blood circulation. This inadequate circulation leads to a significant drop in the amount of oxygen that reaches vital organs.
The brain and heart are particularly vulnerable to these drops in oxygen levels. Without immediate treatment to restore a normal rhythm, the lack of oxygen can cause irreversible damage to these organs, leading to sudden cardiac death. This outcome highlights the critical importance of maintaining a regular heart rhythm for overall health and survival.
Why does irregular heart rate result in cough?
The cough triggered by fluid buildup in the lungs, known as pulmonary edema, happens because the body instinctively responds to the presence of excess fluid in the airways. When the heart can’t pump blood effectively, as is the case with congestive heart failure, fluid leaks into the lung tissue from the blood vessels.
This leakage is the body’s attempt to manage the imbalance, but it inadvertently leads to congestion in the lungs. To clear this congestion and maintain open airways for breathing, the body initiates a cough reflex. This mechanism is both a protective response to prevent fluid from further inhibiting oxygen exchange in the lungs and a symptom signaling underlying cardiac issues that need attention.
Why does irregular heartbeat results in blood clots?
A blood clot forms as a direct consequence of disrupted blood flow, primarily due to irregular heart rhythms such as those seen in ARVC (Arrhythmogenic Right Ventricular Cardiomyopathy). When the heart’s rhythm is off, blood doesn’t circulate smoothly or swiftly enough.
This sluggish or turbulent flow allows blood cells to aggregate more easily, forming clots. These clots can pose severe health risks, including blocking major arteries that can lead to strokes or heart attacks. Thus, maintaining a regular heart rhythm isn’t just about avoiding discomfort; it’s vital for preventing potentially life-threatening complications like thrombus formation.
What is meant by Turbulent Blood Flow?
In the context of fluid dynamics, when blood flow becomes turbulent, it no longer moves smoothly along the blood vessels. This turbulence can occur for various reasons, including irregular heart rates or obstructions within the vessels themselves. Normally, blood flows in a laminar fashion, meaning layers of blood slide over one another in a streamlined manner.
However, when blood flow is turbulent, these layers mix chaotically, creating an environment conducive to clot formation. The erratic movement disrupts the normal anticoagulant properties of blood, allowing platelets and coagulation factors to cluster together more easily. This aggregation can lead to the formation of a blood clot, or thrombus, potentially blocking blood flow to critical areas of the body, resulting in serious health risks.
Thank You
We extend our deepest gratitude to our readers for spending time with our content. Your engagement and curiosity drive us to continuously deliver valuable and precise information. We are fully committed to maintaining the accuracy of our articles and welcome any comments, corrections, or feedback from subject matter experts and enthusiasts alike in the field of veterinary science and pet health.
Should you find any inaccuracies or have insights that could enrich our discussion, please do not hesitate to reach out. Together, we can ensure that our content remains a trustworthy and beneficial resource for all.
Fun Facts
We add additional information here after an engaging discussion with my mother on how the brain can actually operate independently from the body.
Fun facts after I found out that the heart could beat on it’s own independantly of the brain. Many thanks for Dr. Farida Ithnin for this eye-opening revelation!
You can check out her LinkedIn too!
Why is the heart beating independently important for organ transplant?
The heart’s ability to beat independently of the brain is due to a remarkable feature known as the Sinoatrial (SA) Node. Often referred to as the heart’s natural pacemaker, the SA node generates electrical impulses that initiate each heartbeat, maintaining a steady rhythm that ensures blood is continuously pumped throughout the body.
This autonomous function is crucial, especially in scenarios like organ transplants, as it allows the heart to continue beating even when not directly controlled by the brain. Under controlled conditions with mechanical ventilation, this independent beating is a linchpin in keeping organs viable for transplantation, ensuring they remain oxygenated and nourished by the blood flow despite the donor’s brain activity ceasing.

In the subsequent sections, we will explore how this physiological principle is instrumental in organ preservation and the broader implications it has for medical science, especially in life-saving procedures.
Importance of Mechanical Ventilation in Supporting Brain Dead Patients Awaiting Organ Donation
When a person is declared brain dead, it means that there is no measurable brain function, and the condition is irreversible. Despite the cessation of brain activity, the heart can continue to beat, and organs can remain functional for a short period if mechanical support is provided. Mechanical ventilation plays a crucial role in this context by ensuring the flow of oxygenated blood to the organs. The ventilator operates as an artificial breathing apparatus, stepping in to manage the respiratory functions that the brain, once deceased, can no longer oversee. This is crucial because, unlike the heart which can continue to pump blood autonomously for a time, the brain directly controls breathing.
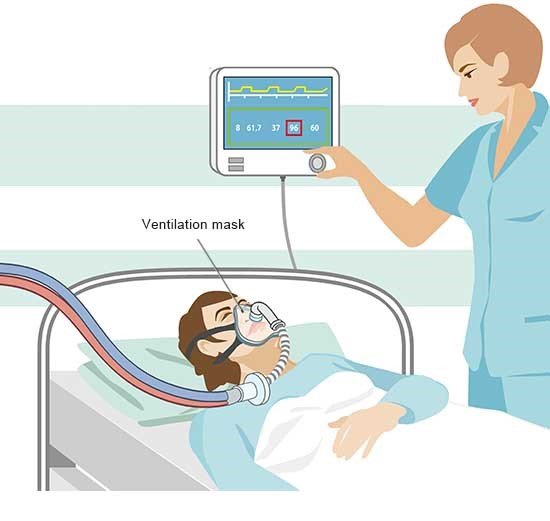
In the absence of this control, the ventilator becomes indispensable in maintaining the vital exchange of oxygen and carbon dioxide.This artificial respiration ensures that oxygen is delivered to the blood, which the still-functioning heart then pumps throughout the body, keeping the organs viable for transplant. This process highlights the critical importance of maintaining oxygenation to the organs in brain-dead patients, enabling the possibility of saving others’ lives through organ donation.
Why must organ donors be declared brain dead with hospital support?
The necessity of the brain stem for breathing highlights a fundamental aspect of human physiology. This critical region of the brain relays signals to the body to initiate the intricate process of respiration, a process vital for life. The brain stem’s role in managing the rhythm of breathing underscores the interconnectedness of our body’s systems. When the brain stem ceases to function due to severe injury or death, the body cannot perform the automatic act of breathing, leading to a cessation of oxygen intake and carbon dioxide expulsion.

This interruption has profound implications for organ health. Oxygen is crucial for the survival and function of cells; without it, organs begin to deteriorate almost immediately. This deterioration limits the window in which organs can be considered viable for transplant, underlining the urgency of maintaining oxygenation in potential organ donors. Thus, the dependency of breathing on the brain stem directly influences the viability of organs for transplantation, emphasizing the need for mechanical support in preserving life-saving transplant opportunities.
Thanks, Peace and Love!
Shafik Walakaka