Navigating the Waters of MDR1 Mutation: A Guide for Dog Owners
In the world of dog breeding and care, understanding genetic conditions is crucial for ensuring the health and well-being of our beloved pets. One such condition that has garnered attention over the years, particularly among Australian Shepherds, Collies, and other sheepdog breeds, is the MDR1 mutation. This genetic quirk can turn common medications into potential threats, making informed care a must for affected dogs.
Introduction to MDR1
The MDR1 (Multi-Drug Resistance 1) gene mutation impacts a dog’s ability to process certain medications. Originally discovered in Collies, it’s now known to affect a range of breeds. Essentially, dogs with this mutation may experience severe, even fatal, reactions to drugs that are otherwise safe.
The Cause: A Genetic Anomaly
At the heart of MDR1 is a glitch in the gene responsible for encoding P-Glycoprotein. This protein plays a critical role in pumping toxins out of cells, particularly in the brain. When its function is compromised, drugs meant to be expelled accumulate, posing a significant risk.
Medications to Watch and Implications of MDR1
Some of the drugs that can cause issues in dogs with the MDR1 mutation include:
- Ivermectin: Often used for parasite control.
- Loperamide: A common anti-diarrheal.
- Acepromazine: Used for sedation.
- Chemotherapy drugs: Such as Vincristine, Doxorubicin, and others.
- Cardiac drugs: Including Digoxin.
For detailed description of the location where toxins build up and implications, please check out this section of the article!
The inability to pump out toxins means affected dogs have a limited list of safe medications, complicating treatment plans for common ailments.
Management and Treatment
While there is no cure for the MDR1 mutation, genetic testing can identify carriers, allowing for careful medication management. Awareness among vets and owners is crucial, as is the selection of alternative treatments when necessary.
Ethical Breeding Practices
Given the prevalence of MDR1, particularly in Collies where up to 50% may be affected, ethical breeding practices are paramount. Responsible breeders test for the mutation and make informed decisions to prevent passing it on, ensuring the health of future generations.
The Path Forward
For dog owners, especially those with breeds susceptible to the MDR1 mutation, the key to managing this condition lies in education, awareness, and proactive health management. By staying informed and working closely with knowledgeable veterinarians, owners can ensure their pets lead safe, healthy lives despite genetic challenges.
In Summary

The MDR1 mutation presents a unique set of challenges, but with the right knowledge and approach, managing these risks is entirely possible. By prioritizing genetic testing, medication awareness, and ethical breeding practices, we can protect our pets from potential harm, ensuring they live full, happy lives.
Navigating the complexities of conditions like the MDR1 mutation may seem daunting, but it’s a testament to the bond between dogs and their owners. Through understanding and vigilance, we can overcome these challenges together, reinforcing the love and care we share with our four-legged companions.
For anyone looking to deepen their understanding or share their experiences with MDR1, remember, this platform is a community of learning and support. Your insights and stories are invaluable as we all strive to ensure the best for our beloved pets.
A Deeper Look at P-Glycoprotein
To have a better appreciation of MDR1, it’s essential to understand the fundamentals of P-Glycoprotein. This vital protein acts as a biological bouncer, guarding cells by pumping out foreign substances that could pose a threat, including many drugs.

Found in the lining of the brain, intestines, liver, and kidneys, its role is crucial in maintaining the body’s defense mechanisms against potentially harmful chemicals. The efficiency of P-Glycoprotein not only affects the absorption and distribution of medications but also their elimination from the body.
Hence, when the function of this protein is compromised due to the MDR1 mutation, it results in an accumulation of drugs within the brain and other critical organs, leading to increased sensitivity or adverse reactions. Understanding P-Glycoprotein’s role illuminates why the MDR1 mutation has such significant implications for affected dogs and the care they require.

Illustration of the increased brain penetration of cortisol in the absence of P-gp (MDR1−/− mutant dogs) and the subsequent suppression of the HPA axis
ABCB1 Gene
The ABCB1 gene is responsible for the production of P-Glycoprotein. It encodes for the protein that plays a pivotal role in the body’s ability to protect itself against toxic substances. When functioning normally, the P-Glycoprotein facilitates the efflux of various substances, including drugs, out of cells to maintain a balance and prevent potential harm to organs such as the brain, liver, and kidneys.
Mutations in the ABCB1 gene, like the MDR1 mutation, lead to a defective or insufficient production of P-Glycoprotein. This deficiency compromises the body’s defense mechanism, rendering it unable to effectively expel certain drugs and toxins. Consequently, affected animals, particularly those breeds with a high incidence of the MDR1 mutation, face serious health risks when exposed to standard doses of medications that are otherwise safe for animals without the mutation.
The intricate relationship between the ABCB1 gene and P-Glycoprotein underscores the critical need for genetic testing and personalized medical management for at-risk breeds.
The Efflux Pump Mechanism of P-Glycoprotein
P-Glycoprotein functions as an efflux pump through a complex process that hinges on its ability to bind and hydrolyze ATP, the energy currency of the cell. This ATPase activity is directly involved in the translocation of substrates across the cell membrane.
Here’s how it works in a nutshell:
P-Glycoprotein binds to its substrate—the compound it aims to expel from the cell—along with ATP. The hydrolysis of ATP provides the necessary energy for a conformational change in the protein structure, effectively flipping the substrate from the inner to the outer leaflet of the cell membrane. Following the release of the substrate outside the cell, ADP is released, and a new ATP molecule binds, readying the pump for another cycle.

The specificity of P-Glycoprotein for substrates is both broad and somewhat selective, enabling it to recognize and transport a wide variety of compounds, including drugs, toxins, and metabolites. This substrate recognition is thought to occur through multiple drug-binding sites, allowing P-Glycoprotein to interact with structurally diverse molecules. Factors that influence this specificity include the size, charge, and hydrophobicity of potential substrates. This multiplicity in substrate recognition is a key factor in P-Glycoprotein’s role in drug resistance, as it can lead to the efflux of a wide array of therapeutic agents, reducing their efficacy by lowering their intracellular concentrations.
Equilibrium and Toxin Efflux
The body maintains a complex equilibrium that directly impacts the efficiency of the P-Glycoprotein efflux pump in expelling toxins. This equilibrium is a sophisticated balancing act, influenced by an array of factors including the presence of substrates, ATP availability, and cellular conditions.
In healthy dogs, this system is finely tuned to ensure that toxins are efficiently pumped out of cells, keeping their concentration at levels that are non-toxic. The equilibrium ensures that despite the constant exposure to potentially harmful substances, a dog’s internal environment remains stable and safe, thanks to the vigilant action of the P-Glycoprotein efflux pump. This is crucial in preserving the health and well-being of the animal, highlighting the essential role of the efflux pump mechanism in detoxification processes.
Where do the Toxins Go?
Once expelled by the P-Glycoprotein pump, the destination and fate of toxins depend on the chemical nature of the substance being effluxed. Generally, these substances are transported into the bloodstream or extracellular spaces. From there, they may be excreted from the body through routes such as urine or feces, or they could be subjected to further metabolism by other organs or cells to reduce their toxicity.

For instance, a metabolite effluxed by liver cells into the bloodstream can be transported to the kidneys, where it is further filtered and eventually excreted in the urine. This multi-step detoxification process underscores the integrated function of different organs and cells in maintaining the body’s internal equilibrium and defending against potential toxic harm.
The ABCB1 Gene Mutation and Its Effects
The mutation in question occurs within the ABCB1 gene, which is responsible for encoding the structure of the P-Glycoprotein. When a mutation occurs, it leads to alterations in the protein’s structure, which in turn affects its efficiency as an efflux pump. This is the underlying reason for the observed deficiencies in toxin expulsion, ultimately leading to an accumulation of potentially harmful substances in the body. Depending on the specific chemicals involved and their targets, this accumulation can result in varying degrees of toxicity.
For example, one well-known chemical sensitive to the ABCB1 mutation is Ivermectin, a common antiparasitic medication. In dogs with the mutated ABCB1 gene, Ivermectin can cross the blood-brain barrier and accumulate in the central nervous system, leading to severe neurotoxicity. This serves as a clear illustration of how genetic factors can directly influence the efficacy of detoxification processes and highlight the importance of understanding an individual’s genetic makeup when prescribing medications or assessing environmental exposures.
Taylor Swift Might Agree: Two Healthy ABCB1 Genes Are Better Than One
Adding a touch of light-heartedness to a rather technical subject, it’s somewhat akin to what Taylor Swift might say about relationships but in the context of genetics — having two healthy ABCB1 genes certainly beats having just one. Just as Swift’s lyrics often highlight the importance of harmony and understanding in a relationship, the harmony between two functioning ABCB1 genes is crucial for maintaining the body’s ability to fend off toxicity.

Jokes aside, if both copies of the ABCB1 gene harbor the MDR1 mutation, the repercussions on the P-Glycoprotein’s functionality are notably more severe. With both efflux pumps compromised, an individual’s capacity to expel various toxins and drugs from cells becomes significantly diminished. This dual mutation can escalate the risk of adverse reactions to medications like Ivermectin and potentially increase vulnerability to environmental toxins. Thus, while the notion of “two is better than one” can evoke a chuckle, especially when borrowing from pop culture, it underscores a profound truth about genetic resilience and the complexities of our biological defense mechanisms.
Drugs Affected by MDR1 Mutation
It’s vital to understand that the list provided here does not cover all the medications affected by the MDR1 mutation. The interactions between genetics and medication can be complex, and new findings are frequently reported. Therefore, if your pet is diagnosed with this genetic variation, it’s crucial to consult with your veterinarian for a detailed and personalized assessment. They can offer the most current advice on which medications to avoid and suggest safe alternatives, ensuring your pet’s health and safety.
Ivermectin:
Ivermectin is primarily used in dogs for the prevention and treatment of heartworm and certain types of mites and lice. It works by paralyzing and killing parasites, offering a highly effective solution to managing these conditions.

Location of Toxic Buildup: Primarily in the central nervous system, including the brain and spinal cord.
Mechanism: Ivermectin readily crosses the blood-brain barrier and accumulates in high concentrations in the brain tissue. Dogs with the MDR1 mutation lack functional P-glycoprotein at the blood-brain barrier, leading to impaired drug efflux and toxic buildup in the brain.
Implication: Neurological symptoms such as tremors, seizures, and coma may occur due to ivermectin toxicity in MDR1-affected dogs.
Loperamide:
Loperamide is primarily used in dogs to manage symptoms of acute and chronic diarrhea. It acts by slowing down the movement of the intestines, allowing for the absorption of more water and nutrients, which helps in firming up stools.

Location of Toxic Buildup: Primarily affects the gastrointestinal tract and the central nervous system.
Mechanism: Loperamide acts by slowing the movement of the intestines, allowing for increased absorption of fluid and nutrients. In dogs with MDR1 mutation, loperamide can excessively accumulate in the central nervous system due to impaired efflux, crossing the blood-brain barrier.
Implication: Excessive accumulation may lead to severe constipation, sedation, or even life-threatening respiratory depression in affected animals.
Acepromazine:
Acepromazine is commonly used as a sedative and tranquilizer for dogs undergoing stressful situations, such as vet visits or grooming sessions. It helps to calm anxious dogs, making it easier to handle them during procedures that might be stressful.

Location of Toxic Buildup: Central nervous system, specifically affecting brain function.
Mechanism: Acepromazine is a tranquilizer used widely in veterinary medicine. The MDR1 mutation impedes the drug’s efflux from the brain, leading to prolonged sedative effects.
Implication: Animals with this mutation may experience exaggerated sedation, profound hypotension, or respiratory depression, necessitating lower doses or alternative medications.
Vincristine:
Vincristine is primarily used in dogs as part of chemotherapy protocols to treat various types of cancer, including lymphoma and leukemia. It works by inhibiting cell division, which is crucial in slowing the growth and spread of cancer cells.
Location of Toxic Buildup: Acts systemically but adverse effects are often noted in rapidly dividing cells such as those of the gastrointestinal tract and bone marrow.
Mechanism: Vincristine is a chemotherapy agent that inhibits cancer cell growth. Dogs with the MDR1 mutation have a decreased ability to remove vincristine from their cells leading to increased toxicity.
Implication: This can result in prolonged neutropenia (low neutrophil count), which significantly increases the risk of infection, as well as severe gastrointestinal toxicity.
Doxorubicin:
Doxorubicin is commonly used in veterinary medicine to treat a variety of cancers in dogs, such as lymphoma, leukemia, and various solid tumors. It operates as an anthracycline antibiotic that interferes with the replication of cancer cells, thereby slowing or stopping tumor growth.

Location of Toxic Buildup: Systemically affecting cells, particularly those of the heart and bone marrow.
Mechanism: Doxorubicin is an anthracycline antibiotic used as a chemotherapy drug. The inability to efficiently expel doxorubicin from the cells due to the MDR1 mutation results in enhanced cardiotoxicity and myelosuppression.
Implication: Affected dogs may show signs of congestive heart failure or severe bone marrow suppression, highlighting the need for adjusted dosing or alternative therapies.
Paclitaxel:
Paclitaxel is utilized in veterinary oncology primarily for its efficacy in treating solid tumors, including mammary carcinoma and non-small cell lung cancer in dogs. It works by stabilizing microtubules, thereby inhibiting cell division and inducing cancer cell death.

Location of Toxic Buildup: Acts on microtubules affecting cell division, impacting various tissues but notably causing neurotoxicity.
Mechanism: Paclitaxel prevents the normal breakdown of microtubules during cell division. MDR1 mutation reduces the ability to expel paclitaxel, leading to its accumulation and increased side effects.
Implication: This accumulation can cause severe peripheral neuropathy, characterized by weakness, pain, and sensory changes, necessitating careful monitoring and dose adjustment.
Etoposide:
Etoposide is commonly used in the treatment of various types of cancer in dogs, particularly for lymphoma and leukemia. It acts by inhibiting the enzyme topoisomerase II, leading to DNA damage and cancer cell death, but requires careful dosage management due to its narrow therapeutic range.

Location of Toxic Buildup: Primarily impacts the bone marrow but can affect all rapidly dividing cells.
Mechanism: Etoposide interferes with DNA synthesis, leading to cell death. In animals with the MDR1 mutation, etoposide’s removal from cells is hindered, raising its cytotoxic effects.
Implication: The result can be excessive bone marrow suppression, resulting in leukopenia (reduced white blood cell count), increasing the risk of infections.
Digoxin:
Digoxin is utilized in dogs for treating heart conditions, specifically congestive heart failure and certain types of arrhythmias. It improves heart function by increasing the force of cardiac contractions and regulating heart rate.
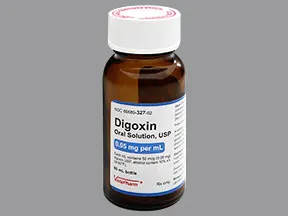
Location of Toxic Buildup: Primarily affects the myocardium (heart muscle).
Mechanism: Digoxin is used to treat heart failure and arrhythmias. The MDR1 mutation can limit the drug’s efflux from cardiac cells, allowing digoxin to accumulate to toxic levels.
Implication: Toxicity can result in fatal arrhythmias, necessitating lower doses and careful monitoring of serum drug levels in affected animals.
Morphine:
Morphine is primarily used in dogs for its potent analgesic properties, providing relief from severe pain. Additionally, it can be used as a sedative to calm dogs undergoing stressful procedures or surgeries.
Location of Toxic Buildup: Central nervous system and gastrointestinal tract.
Mechanism: Morphine, a potent analgesic, impacts opioid receptors. In dogs with MDR1 mutation, the drug’s efflux from the brain is compromised, leading to prolonged and intensified effects.
Implication: This can result in excessive sedation, respiratory depression, and delayed gastrointestinal transit, which could be life-threatening, highlighting the importance of dose adjustment or alternative pain management strategies.
What about Topical Application?
Even though there’s less documentation on the effects of topical medications in dogs with the MDR1 mutation, caution is still the order of the day. The substrates like permethrin, imidacloprid, corticosteroids, and topical anesthetics, though applied externally, can still enter the systemic circulation. Especially in animals with compromised skin barrier function or when used over large surface areas, the absorption might increase.

Given the role of P-Glycoprotein in pumping these substances out of cells, animals with the MDR1 mutation could potentially experience increased exposure to these compounds. This elevates the risk of systemic side effects, affirming the necessity of careful consideration and veterinary consultation when choosing topical treatments for dogs known to carry the MDR1 mutation.
Thank You!
I hope this exploration into the intricacies of the MDR1 mutation and its impact on toxin efflux by P-Glycoprotein has been as enlightening for you as it has been for me. Understanding these fundamentals is crucial for the well-being of our furry companions, especially when it comes to managing their health and treatment options effectively. I’ve thoroughly enjoyed sharing this knowledge with you, and as always, should there be any inaccuracies or areas for clarification, please don’t hesitate to highlight them. Here’s to the health and happiness of our pets!

Thanks, Peace and Love!
Shafik Walakaka